Understanding and Minimizing Radiation Exposure
During Fluoroscopy-Guided Injections
Fluoroscopy is an invaluable tool in interventional and naturopathic regenerative pain management. Its ability to provide real-time imaging during procedures makes it the gold standard for precision-guided spine injections and other interventional techniques. This advanced imaging modality enables practitioners to deliver targeted treatments with unparalleled accuracy, minimizing risks and maximizing patient outcomes.
While fluoroscopy involves exposure to ionizing radiation, the benefits it provides in terms of safety, efficacy, and procedural success far outweigh the risks, especially when appropriate safety measures are implemented. In this article, we’ll explore why fluoroscopy is essential in interventional and regenerative pain practices, discuss radiation exposure, and highlight the strategies our practice employs to minimize risks.
Why Fluoroscopy is the Gold Standard
Fluoroscopy is considered the gold standard for several interventional procedures, including:
- Spine Injections: Accurate placement of medications or regenerative therapies into the epidural space, facet joints, or sacroiliac joints requires the precise visualization that fluoroscopy provides.
- Nerve Blocks: Fluoroscopy ensures precise targeting of specific nerves, reducing the risk of complications and increasing therapeutic efficacy.
- Joint Injections: For deeper joints like the hip or shoulder, fluoroscopy ensures accurate placement of treatments, particularly when regenerative therapies such as platelet-rich plasma (PRP) or stem cells are used.
- Radiofrequency Ablation (RFA): Fluoroscopy guides electrode placement for nerve ablation, ensuring optimal outcomes.
The ability to visualize anatomical structures in real time makes fluoroscopy an indispensable tool, particularly in complex cases or when working with intricate anatomy like the spine.
Fluoroscopy in Naturopathic Interventional and Regenerative Medicine
Fluoroscopy is a cornerstone of our naturopathic interventional and regenerative pain management practice. By enabling precise, real-time visualization, fluoroscopy enhances the efficacy of treatments such as:
- Epidural Steroid Injections for pain relief and inflammation reduction of spinal nerves.
- Facet Joint Injections to improve mobility and reduce spinal joint pain.
- Sacroiliac Joint Injections to address lower back pain.
- Regenerative Therapies (e.g., PRP, mFat, Donor Tissue) in joints and soft tissues for healing and pain relief.
This advanced imaging modality ensures that we can deliver targeted treatments safely and effectively, empowering our patients to achieve long-term relief and improved function.
Radiation Exposure in Fluoroscopy-Guided Injections
Fluoroscopy uses X-ray technology to provide real-time imaging, which involves exposure to ionizing radiation. The amount of radiation varies depending on the procedure’s duration, the imaging system’s settings, and patient anatomy. Radiation is measured in millisieverts (mSv), a unit that quantifies the biological effects of ionizing radiation.
For perspective, the average dose from a fluoroscopy-guided injection ranges from 0.1-0.5 mSv, depending on the complexity of the procedure. This is comparable to a standard chest X-ray (~0.1 mSv)
Understanding Radiation Units Used in Fluoroscopy
Understanding radiation exposure in terms of milligray (mGy), millirem (mrem), and millisievert (mSv) contextualizes its use and highlights the strategies we employ to minimize risks for patients and providers.Fluoroscopy uses X-rays to provide live imaging, and the amount of radiation exposure varies based on procedure duration and complexity.
Conversion and Context of Units
- Milligray (mGy): Measures the absorbed dose of radiation.
- Millisievert (mSv): Accounts for biological effects and tissue sensitivity; 1 mSv ≈ 1 mGy for X-rays.
- Millirem (mrem): A smaller unit commonly used in annual dose reports, where 1 mSv = 100 mrem.
Deep Dose Equivalent (DDE): Measures the radiation dose absorbed 1 cm beneath the skin surface, representing exposure to internal organs and deep tissues.
Eye Dose Equivalent (EDE): Specific to the lens of the eye, this measurement assesses scatter radiation affecting the eyes, a critical concern for healthcare workers.
Shallow Dose Equivalent (SDE): Measures radiation absorbed at the skin’s surface (0.007 cm depth), representing exposure to superficial tissues.
| Radiation Dose for Fluoroscopy-Guided Injections |
|---|
| Absorbed Dose: 50–200 mGy (0.5–2 mSv or 50–200 mrem)** |
Comparing Imaging Modalities and Everyday Exposure
| Imaging/Exposure | Absorbed Dose (mGy) | Effective Dose (mSv) | Effective Dose (mrem) |
|---|---|---|---|
| Fluoroscopy-Guided Injection | 50–200 mGy | 0.5–2 mSv | 50–200 mrem |
| Chest X-ray | ~10 mGy | ~0.1 mSv | ~10 mrem |
| Mammogram | ~400 mGy | ~0.4 mSv | ~40 mrem |
| Abdominal CT Scan | ~1,000–3,000 mGy | 8–10 mSv | 800–1,000 mrem |
| Low-Dose CT (SimonMed) | ~150 mGy | ~1.4 mSv | ~140 mrem |
| MRI (no ionizing radiation) | 0 mGy | 0 mSv | 0 mrem |
| Ultrasound (no ionizing radiation) | 0 mGy | 0 mSv | 0 mrem |
| Natural Background Radiation | ~300 mGy/year | ~3 mSv/year | ~300 mrem/year |
| Round-Trip Flight (Cross-Country) | ~3–5 mGy | ~0.03–0.05 mSv | ~3–5 mrem |
This comparison illustrates that radiation exposure from fluoroscopy-guided injections is relatively low and comparable to everyday exposures like natural background radiation or a short flight.
Annual Radiation Limits and Safety for Pain Management Patients
| Dose Type | Annual Occupational Limit | Annual Public Limit | Limit for Patients Undergoing Pain Management Treatments |
|---|---|---|---|
| Deep Dose Equivalent (DDE) | 50 mSv (5,000 mrem or ~50 mGy) | 1 mSv (1,000 mrem or ~1 mGy) | Varies; typically 5–10 mSv/year (5,000–10,000 mrem) depending on treatment frequency |
| Eye Dose Equivalent (EDE) | 150 mSv (15,000 mrem or ~150 mGy) | 1 mSv (1,000 mrem or ~1 mGy) | Not directly relevant unless frequent eye-focused imaging occurs |
| Shallow Dose Equivalent (SDE) | 500 mSv (50,000 mrem or ~500 mGy) | 1 mSv (1,000 mrem or ~1 mGy) | Not typically applicable in localized pain management treatments |
Key Points:
- mSv and mGy Relationship: For X-rays (used in fluoroscopy), 1 mSv ≈ 1 mGy, but biological weighting for tissue sensitivity varies.
- Conversion to mrem: 1 mSv = 100 mrem, which explains the larger numerical values when expressed in mrem.
Tissue Sensitivity Dictates Limits: Different tissues/organs have different radiation sensitivities. Eye tissues are primarily at risk of cataracts, requiring a higher threshold than deep tissues, which are at risk for cancers.
mSv vs. mrem Units: Both mSv and mrem measure dose equivalence, but they are used differently in contexts. Regulations in mSv often directly relate to biological effects, while mrem is a smaller unit used for annual occupational reporting in many practices.
Health Risks Above 50 mSv:
Studies indicate that cumulative radiation doses exceeding 50 mSv may slightly increase the risk of cancer and other adverse health effects, particularly if exposure is chronic or involves high-dose events. Radiation above these levels has been associated with an increased risk of leukemia, thyroid cancer, and cataracts, especially in healthcare professionals without adequate protection.
These limits underscore the importance of minimizing exposure during medical procedures to protect both patients and healthcare providers
Adjusted Limits for Patients Undergoing Pain Management Treatments
For patients receiving fluoroscopy-guided injections as part of their pain management plan, the standard 1 mSv/year public exposure limit may not apply. This is because the medical necessity and benefits of treatment outweigh the minimal risks of additional radiation exposure. While public limits are designed for incidental or environmental exposure, the radiation received during medically necessary procedures is carefully managed to remain within safe thresholds.
Typical Exposure in Pain Management Treatments:
- Patients receiving occasional fluoroscopy-guided injections (e.g., epidural steroid injections, facet joint injections) typically remain well under 5 mSv/year.
- For those requiring more frequent interventions, cumulative exposure may range between 5–10 mSv/year but still remains far below occupational limits of 50 mSv/year.
Why the Benefits Outweigh the Risks
Low Overall Risk:
- For pain management patients, the radiation exposure from a single fluoroscopy-guided injection (0.1–0.5 mSv or 50–200 mrem) is minimal and comparable to natural background radiation or a short flight.
- Even with multiple treatments, exposure remains far below thresholds associated with significant health risks (e.g., 50 mSv/year for occupational workers or 100 mSv cumulative lifetime for increased cancer risk).
Improved Quality of Life:
- Fluoroscopy-guided injections offer precise and effective pain relief, reducing inflammation, restoring mobility, and improving quality of life for patients with chronic pain conditions.
- These benefits far outweigh the minimal theoretical risks of low-dose radiation exposure.
Risk-Benefit Considerations:
- Risks: Theoretical increase in cancer risk with cumulative radiation doses exceeding 100 mSv (10,000 mrem) over a lifetime.
- Benefits: Targeted treatments lead to faster recovery, reduced reliance on systemic medications, and long-term pain relief.
Strategies to Minimize Radiation Exposure
Adhering to Arizona Radiation Safety Guidelines
In Arizona, practitioners must comply with strict guidelines to protect both patients and healthcare providers from unnecessary radiation exposure. Ensuring the proper functioning of fluoroscopic equipment and maintaining accurate radiation dose tracking are fundamental.Employment of Experienced Radiologic Technologists
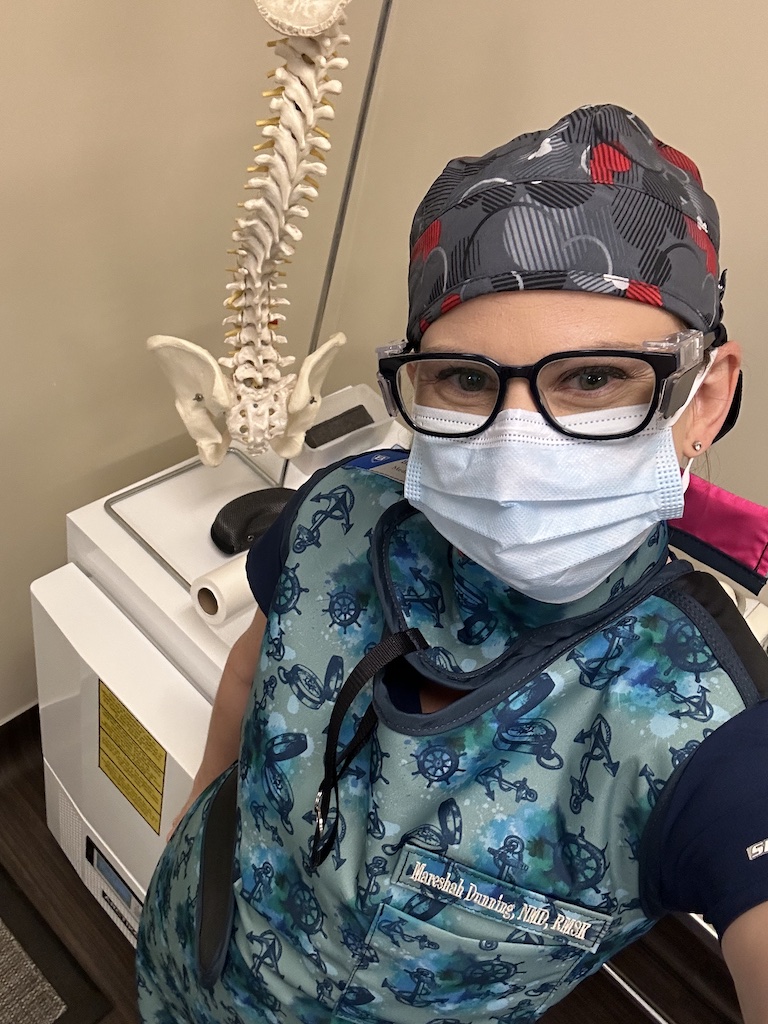
At the Neil Riordan Center for Regenerative medicine where my practice is based out of, employs a highly skilled radiologic technologist who ensures proper equipment settings, minimizes unnecessary exposure, and monitors compliance with state and federal radiation safety guidelines. They optimize imaging parameters, adjust fluoroscopy settings, and ensure proper use of lead shielding for all procedures.
Wearing Appropriate Lead Protection
Lead aprons, thyroid shields, and leaded eyewear are critical protective measures. Lead glasses, for instance, significantly reduce the risk of cataracts and radiation-induced eye damage, which are potential long-term complications for practitioners frequently exposed to scattered radiation.Maximizing Distance from the Radiation Source
The inverse square law governs radiation exposure: doubling the distance from the radiation source reduces exposure by a factor of four. Strategically positioning oneself at the greatest feasible distance from the source, while maintaining procedural accuracy, is a simple yet effective strategy.
– Standing 6 feet away from the radiation source reduces exposure by up to 75%, compared to being close to the source.
– This principle is utilized whenever feasible, while maintaining precision in procedures.Minimizing Fluoroscopy Time
We practice low-dose, intermittent fluoroscopy, which minimizes radiation while maintaining diagnostic accuracy. Using the lowest necessary fluoroscopy settings and limiting imaging time are essential practices. Intermittent fluoroscopy, rather than continuous imaging, reduces radiation exposure without compromising safety or accuracy.Using Collimation and Shielding
Collimating the X-ray beam to focus only on the area of interest reduces radiation scatter. Proper placement of lead shields further protects surrounding tissues.
The Importance of Eye Protection: Lead Glasses
The eyes are particularly sensitive to ionizing radiation. Studies show that frequent exposure can lead to cataracts or other ocular issues. Lead glasses with 0.5 mm Pb equivalence can reduce scatter radiation to the eyes by 65-85%. For practitioners performing frequent fluoroscopy-guided procedures, investing in quality lead glasses is a crucial safety measure.
Research on Radiation and Health Risks
Adverse Events from Radiation Exposure:
- A study in The Lancet found that chronic exposure to occupational radiation, particularly among healthcare workers, is associated with an increased risk of cataracts and cancer.
- Another study highlighted that cumulative doses above 100 mSv could increase the lifetime risk of cancer by approximately 1% .
Radiation Dose and Interventional Procedures:
- The Interventional Radiology Society emphasizes that fluoroscopic procedures are safe when performed with modern low-dose systems and strict adherence to radiation protection guidelines.
- For patients, the risk of adverse effects is negligible when exposure is kept below 50 mSv per year.
Why Radiation Safety Is a Priority
Fluoroscopy is a cornerstone of our practice, enabling us to deliver precise, effective treatments that significantly improve patient outcomes. However, safety is non-negotiable. With a skilled radiologic technologist, state-of-the-art equipment, and strict adherence to Arizona’s radiation safety guidelines, we protect both patients and staff.
By maintaining a strong commitment to radiation safety, we ensure that the benefits of fluoroscopy-guided treatments far outweigh any risks, empowering our patients to regain function and quality of life.
References
- Dauer LT, Thornton RH, Hay JL, Balter S. Discouraging physicians and patients from using lead shielding for radiation protection. Health Phys. 2021;120(4):441-444. doi:10.1097/HP.0000000000001412
- Dauer LT, et al. Cumulative Radiation Dose in Interventional Pain Management: Risks and Recommendations. Health Physics. 2021;120(4):441-446. doi:10.1097/HP.0000000000001412.
- Bushberg JT, Seibert JA, Leidholdt EM Jr, Boone JM. The Essential Physics of Medical Imaging. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.
- Vano E, et al. Radiation-Induced Cataract Risk in Interventional Radiology. The Lancet. 2020;375(2):306-312. doi:10.1016/j.lancet.2020.02.001.
- Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: A catalog. Radiology. 2008;248(1):254-263. doi:10.1148/radiol.2481071451
- National Council on Radiation Protection and Measurements (NCRP). Ionizing Radiation Exposure of the Population of the United States. NCRP Report No. 160. Bethesda, MD: NCRP; 2009.
- Interventional Radiology Society. Radiation Safety in Interventional Procedures. Available at: www.sirweb.org.
U.S. Nuclear Regulatory Commission. Doses in Our Daily Lives. Available at: https://www.nrc.gov/about-nrc/radiation/around-us/doses-daily-lives.html. Accessed November 26, 2024.
SimonMed Imaging. Low-Dose CT Scan. Available at: https://www.simonmed.com/services/ct-scan/. Accessed November 26, 2024.
U.S. Nuclear Regulatory Commission. Backgrounder on Biological Effects of Radiation. Available at: https://www.nrc.gov/reading-rm/doc-collections/fact-sheets/bio-effects-radiation.html. Accessed November 26, 2024.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
